The AAMD Board of Directors would like to thank everyone who reviewed and commented on the draft updated Scope of Practice of a Medical Dosimetrist. All comments are being sent to the Scope of Practice Task Group for consideration. It is anticipated that the final document will be presented at the AAMD 44th Annual Meeting in Anaheim, CA, this June. Questions? Email us at aamd@medicaldosimetry.org
Preamble
The Scope of Practice of a Medical Dosimetrist is designed to assist the Qualified Medical Dosimetrist (QMD) in defining their role in the technical services they provide in patient care. This document also defines the QMD, provides a statement of basic responsibility of the QMD, and addresses their education, certification, continuing education, and maintenance of certification. Statements are included on supervision by and of the QMD; stressing the importance that the QMD be an active participant in the collaborative, team approach to patient care and that effective communication with the radiation oncology team is essential for providing quality patient care and patient safety. (1,2)
In addition, this Scope of Practice is designed to educate professionals in the fields of health care, education, other communities of interest and the general public regarding the expectations of the QMD. (1,2) This document can be used by individual facilities to develop job descriptions and practice parameters.
The Scope of Practice defined in this document is meant to have some flexibility in interpretation and is not intended to be used to establish a legal standard of care. (2) Professionals who use this document must be aware of state and federal laws affecting their practice as well as institutional policies and guidelines, as the intent is not to supersede these laws or affect the interpretation or implementation of such laws. (1)
The American Association of Medical Dosimetrists (AAMD) is an international society established to promote and support the Medical Dosimetry profession. The AAMD is committed to advance the science, education, and professional practice of medical dosimetry. The AAMD periodically reviews and updates the professional practice guidelines for the QMD to help advance the technical services provided by the QMD and to improve the quality of services to patients. In addition, the AAMD provides opportunities for education, a forum for professional interaction and a representative voice in the healthcare community. The Society seeks to promote an ideal of professional conduct to which its members should aspire and endorses the highest standards of patient care. (3)
I. Qualified Medical Dosimetrist (1,2)
A Qualified Medical Dosimetrist is an individual who obtains the basic competency to practice in collaboration with a Radiation Oncologist (RO) and/or a Qualified Medical Physicist (QMP). The individual uses critical thinking and problem-solving skills as well as exercises their discretion and judgment in the performance of medical dosimetry procedures.
It is expected that an individual will hold themselves qualified to practice in Medical Dosimetry only when the knowledge and skills to perform dosimetric tasks has been established. An individual shall be considered eligible to practice if they are certified by the Medical Dosimetrist Certification Board (MDCB).
Effective as of 2017, all United States candidates for MDCB certification will be required to apply as Route 1 candidates holding a Bachelor’s Degree and be graduated from a formal dosimetry program accredited by the Joint Review Committee on Education in Radiologic Technology (JRCERT) by the late application deadline. The American Association of Medical Dosimetrists (AAMD) has fully endorsed this educational level for new candidates in the United States. (2)
The AAMD recommends all personnel practicing in Medical Dosimetry attain, at a minimum, certification provided by the MDCB. Accordingly, the Certified Medical Dosimetrist (CMD) is recognized as the appropriate credential for the QMD. (2)
II. Professional Competence
Professional competence is the habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values and reflection in daily practice for the benefit of the individual and community being served. (1)
III. Statement of Basic Responsibility
The essential responsibility of the QMD is to generate a clinically acceptable treatment plan, utilizing clinical knowledge including, but not limited to, anatomy, physiology, radiation biology and oncology, radiation safety and protection, mathematics, and radiation therapy techniques, physics and technology. The QMD is expected to communicate with the RO during the treatment planning process and participates in communicating the plan to the QMP and to the Radiation Therapist (RT) for implementation. The QMD must maintain a commitment to a high degree of accuracy, attention to detail, and safety. The QMD must use critical thinking skills when performing radiation treatment planning, plan evaluation, recognizing and resolving equipment problems and treatment discrepancies. (1)
IV. Definitions
The Qualified Medical Dosimetrist (QMD) is a member of the radiation oncology team who has a knowledge of the overall characteristics and clinical relevance of radiation oncology in the management of cancer or other radio-responsive conditions, with special expertise in radiation therapy treatment planning. (1,2)
The Practice of Medical Dosimetry is performed by health care professionals responsible for the process of patient data acquisition, radiation treatment planning for the administration of ionizing radiation, and quality management for radiation oncology patients. The QMD may have to ensure accurate transfer of patient information to a number of software, which may include record/ verify systems, surface guidance and/or image guided systems and treatment delivery systems. In addition to the above, the QMD may perform or assist in other duties under the direction of the Board-Certified Radiation Oncologist (RO) and a Qualified Medical Physicist (QMP). (1, 4)
A Board-Certified Radiation Oncologist (RO) denotes a Doctor of Medicine who is licensed to practice their medical specialty and who prescribes and/or utilizes radiological procedures for individuals for the diagnosis or treatment of their ailment. The RO directs and utilizes the services of many interdisciplinary professions. (2,3)
For providing clinical professional services, a Qualified Medical Physicist (QMP) is an individual who is competent to independently provide clinical professional services in one or more of the subfields of medical physics. A QMP is qualified to practice only in the subfields(s) in which they are certified. A QMP must hold a professional medical physics license where required. (2, 3)
QMDs are educated to independently perform duties and complete responsibilities under the direction of a RO and a QMP. (1)
V. Specifics of Practice
This document summarizes the activities that the QMD can undertake based on the individual’s training, qualifications, and demonstration of competence. Each QMD must exercise professional and prudential judgment in determining whether they are educationally prepared and clinically competent to perform a given activity. The QMD understands when to seek guidance and assistance with assigned activities (1).
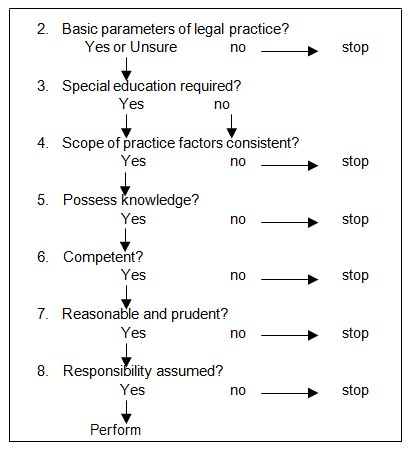
The decision-making model described in Appendix 1, provides rational and logical guidance to QMDs. When these guidelines are used to analyze whether a QMD may perform a task, the conclusion is reached that this act is or is not within the scope of practice of the individual QMD. (1)
QMDs should adhere to the AAMD Code of Ethics and the Ethical Standards of the MDCB. (1,2)
VI. Education and Certification
The AAMD recommends that QMDs entering the field be prepared for this profession by earning the minimum of a baccalaureate degree, completing a Medical Dosimetry educational program accredited by the JRCERT and obtaining certification by the MDCB and continuing education following MDCB’s Maintenance of Certification. (1-3)
The AAMD fully supports the MDCB routes of eligibility change beginning in 2017 that requires all examinees to have a baccalaureate degree and to have graduated from JRCERT accredited medical dosimetry educational program. (4)
VII. Continuing Education / Maintenance of Certification
Radiation oncology is a rapidly changing and technologically-advanced field. It is imperative that the QMD maintain a level of expertise and awareness of changes and advances to remain current in the field.
Maintenance of certification by the MDCB is part of the continuing education of the QMD. Once certified, the QMD is personally and professionally responsible for the maintenance of certification according to the guidelines established by the MDCB. (1,2)
VIII. Supervision (1)
A QMD receives supervision from the RO, QMP, and senior / lead QMDs.
A QMD may supervise other QMDs and other allied health professionals.
IX. Collaboration and Communication (1,2,3)
Collaboration and communication are essential to the process of patient data acquisition, radiation treatment planning, treatment plan evaluation, accurate treatment delivery, and quality management for radiation oncology patients. It is imperative that QMDs actively and openly collaborate and communicate with:
X. The Scope of Practice of the Qualified Medical Dosimetrist Shall include, but is not limited to: (1,2,3)
Decision Making
In addition to the Scope and Standards of Medical Dosimetry Practice, each QMD must exercise professional and prudent judgment in determining whether the performance of a given act is within the scope of practice for which the QMD is clinically competent to perform. The decision-making model, subsequently described, provides rational and logical guidance to QMDs. When these guidelines are used to analyze whether a QMD may perform a task, the conclusion is reached that this act is or is not within the scope of practice. (1) (See Figure 1)
Decision Making Model for Determining the Scope of Practice of a Qualified Medical Dosimetrist
Summary of Decision-Making Model
Preamble
1. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
2. American College of Radiology. ACR - ASTRO Practice Parameter Radiation Oncology, Revised 2018 (CSC/BOC)
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/RadOnc.pdf?la=en
Accessed February 7, 2019.
3. American Association of Medical Dosimetrists.
https://www.medicaldosimetry.org/membership/join/
Accessed February 13, 2019.
I. Qualified Medical Dosimetrist
1. American Association of Medical Dosimetrists. Definition of a Qualified Medical Dosimetrist.
https://www.medicaldosimetry.org/about/definition/
Accessed October 16, 2018.
2. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
II. Professional Competence
1. Epstein, RM, Hundert, EM, Defining and Assessing Professional Competence, Journal of the American Medical Association 2002 January 9; 287(2): 226-235.
https://www.ncbi.nlm.nih.gov/pubmed/11779266
Accessed February 8, 2018.
III. Statement of Basic Responsibility
1. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
IV. Definitions
1. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
2. American College of Radiology, ACR-ASTRO Practice Parameter for Radiation Oncology, Revised 2018 (CSC/BOC).
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/RadOnc.pdf?la=en
Accessed February 13, 2019.
3. American Association of Physicists in Medicine. AAPM Professional / Education /Science Policies; Definition of a Qualified Medical Physicist, August 2018.
https://www.aapm.org/org/policies/details.asp?id=449&type=PP
Accessed February 13, 2019.
4. Medical Dosimetrist Certification Board, MDCB Job Task Analysis November 2018
https://mdcb.org/sites/default/files/images/2019/MDCB Summary_ 2018 JTA.pdf
Accessed February 13, 2019.
V. Specifics of Practice
1. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
2. Medical Dosimetrist Certification Board. Ethical Standards and Ethics Complaint Procedures of the MDCB. Amended August 15, 2011.
https://mdcb.org/about-mdcb/ethical-standards
Accessed February 7, 2018.
VI. Education and Certification
1. American College of Radiology. ACR - ASTRO Practice Parameter for Radiation Oncology, Revised 2018 (CSC/BOC)
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/RadOnc.pdf?la=en
February 13, 2019.
2. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
3. American Association of Medical Dosimetrists. Definition of a Qualified Medical Dosimetrist, 2012.
https://www.medicaldosimetry.org/about/definition/
Accessed February 7, 2018.
4. Medical Dosimetrist Certification Board. Applicant Handbook, 2018.
https://mdcb.org/sites/default/files/documents/2018/Exam Handbook_2018.8_FINAL.pdf
Accessed March 5, 2018.
VII. Continuing Education / Maintenance of Certification
1. Medical Dosimetrist Certification Board. Applicant Handbook, 2018.
https://mdcb.org/sites/default/files/documents/2018/Exam Handbook_2018.8_FINAL.pdf
Accessed March 5, 2018.
2. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
VIII. Supervision
1. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
IX. Collaboration and Communication
1. American Association of Physicists in Medicine. Professional / Education/ Science
AAPM medical physics practice guideline 10.a.: Scope of practice for clinical medical physics
https://aapm.onlinelibrary.wiley.com/doi/full/10.1002/acm2.12469
Accessed February 13, 2019.
2. American College of Radiology, ACR-ASTRO Practice Parameter for Communication:
Radiation Oncology, Revised 2014 (CSC/BOC)
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/Communication-RO.pdf?la=en
Accessed February 13, 2019.
3. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
X. The scope of practice of the Qualified Medical Dosimetrist may include, but is not limited to:
1. American Association of Medical Dosimetrists. Medical Dosimetrists General Job Description, 2011.
https://www.medicaldosimetry.org/about/job-description/
Accessed March 5, 2018.
2. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
3.Medical Dosimetrist Certification Board. MDCB Job Task Analysis November 2018.
https://mdcb.org/sites/default/files/images/2019/MDCB Summary_ 2018 JTA.pdf
Accessed February 13, 2019.
Appendix 1
1. American Association of Medical Dosimetrists. Scope of Practice of a Medical Dosimetrist, 2012.
https://pubs.medicaldosimetry.org/pub/416096BB-F21B-1D03-5673-1987E3E85D0B
Accessed February 7, 2018.
Daniel Bailey, PhD, DABR
Medical Physicist
Department of Radiation Oncology
Northside Hospital Cancer Center
Atlanta, GA
Committee Member
Member, AAPM Subcommittee on the Training and Practice of Medical Dosimetry
AAPM Liaison to AAMD
Paula A. Berner, BS, CMD, FAAMD
Brachytherapy Dosimetrist
Bellaire, TX
AAMD Task Group Chair
Minsong Cao, PhD, DABR
Clinical Associate Professor
Department of Radiation Oncology
University of California, Los Angeles
Los Angeles, CA
Committee Member
Member, AAPM Subcommittee on the Training and Practice of Medical Dosimetry
Shiv Srivastava, PhD
Medical Physicist
University of Arizona Cancer Center
Dignity Health
St. Joseph’s Hospital and Medical Center
Phoenix, AZ
Committee Member
Member, AAPM Subcommittee on the Training and Practice of Medical Dosimetry
Walter L. Tang, MS
Senior Consulting Medical Physicist
MRPC, Inc.
Minneapolis, MN
Committee Member
Chair, AAPM Subcommittee on the Training and Practice of Medical Dosimetry